Dear SurgeonMasters Community,What makes a community special?For me, it’s being around people who genuinely support my best interests. It’s the shared
Continue ReadingBalanced Life! Life improvement strategies for the surgeon who wants more … in 10 minutes – Episode 129
Pump the brakes on your week and take 10 minutes to make your life as a surgeon just a little better…Jeff welcomes to the podcast board-certified
Continue ReadingThe Power of Connection in Physician Wellness
SurgeonMasters believes that connection is essential for wellness and that wellness leads to career fulfillment, joy, and sustainability in
Continue ReadingHero Mindset! Life improvement strategies for the surgeon who wants more … in 10 minutes – Episode 128
Pump the brakes on your week and take 10 minutes to make your life as a surgeon just a little better…Jeff welcomes ENT surgeon and professional coach
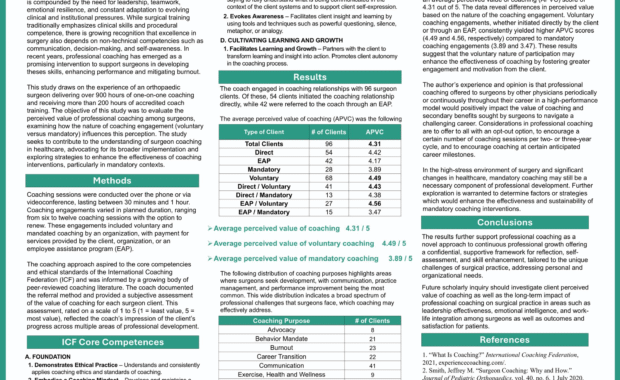
Continue ReadingCutting-Edge Support: The Value of Coaching
Dear Community:Recently, I presented a poster at a surgical leadership conference on the value of coaching. The key takeaway is that voluntary
Continue ReadingThe Value of Coaching for Surgeons
I recently had the honor of presenting data on how surgeons perceive the value of coaching at the American Orthopaedic Association Annual Leadership
Continue ReadingTeam Communication! – Life improvement strategies for the surgeon who wants more … in 10 minutes – Episode 127
Pump the brakes on your week and take 10 minutes to make your life as a surgeon just a little better…Jeff welcomes to the podcast, Quality Improvement
Continue ReadingJeffrey M. Smith, MD, FACS, PCC, to Present Surgeon Coaching Study at the 2025 AOA Leadership Meeting
Minneapolis, MN., June 5, 2025 - SurgeonMasters CEO Jeffrey M. Smith, MD, FACS, PCC, will present the study, Cutting-Edge Support: The Perceived Value
Continue ReadingDefining Your Core Values is Essential
Dear Community,What values define you?It’s not always an easy question to answer.In the rush of clinical demands, administrative pressures, and
Continue Reading